Women are more vulnerable to contracting HIV.
Nov 30, 2022
Women are more vulnerable to contracting HIV.
Nov 30, 2022
Due to factors such as origin and difficulties accessing education and work, the most affected are those living in Sub-Saharan Africa and India.
In mid-1981, the first cases of the Human Immunodeficiency Virus (HIV) were diagnosed worldwide. It started in the United States, and a few months later the first case was reported in Spain, eventually becoming a global pandemic. As noted by the World Health Organization (WHO), this virus attacks the immune system, and treatments can prevent its progression and the development of Acquired Immunodeficiency Syndrome (AIDS).
Since the first cases recorded in the 1980s according to a report by the United Nations’ UNAIDS it is estimated that 78 million people worldwide have contracted HIV, with nearly 37 million active cases currently. In Spain, the Ministry of Health indicates that around 88,700 AIDS cases have been reported in total, and there are currently between 140,000 and 170,000 people living with HIV.
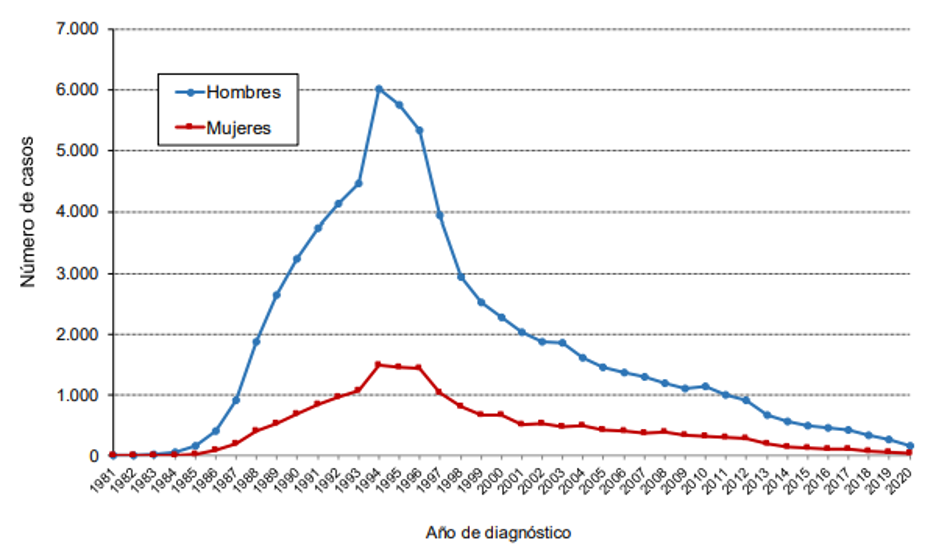
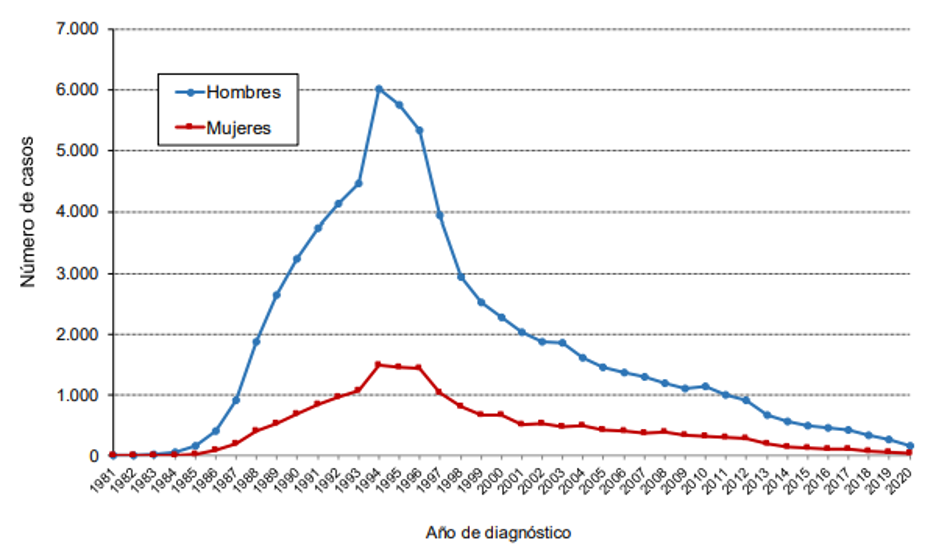
The peak of registered cases occurred in the mid-1990s, and thanks to antiretroviral treatment, the numbers have decreased “progressively,” although this decline has slowed in recent years. Data from the Ministry of Health show 1,925 HIV cases in 2020, with approximately 15% being women under 35 years old the age group with the highest incidence. Medical experts point out that the disease “does not develop the same way in women and men.” In women, complications may include a higher risk of cervical cancer, menstrual cycle problems, increased likelihood of developing osteoporosis, earlier onset of menopause, or risk of transmission to the fetus during pregnancy.
The latest epidemiological surveillance study on HIV and AIDS in Spain shows an increase in virus transmission through heterosexual relationships, with 80.5% of new cases in women occurring in this type of relationship. To curb these figures, work is underway on the Social Pact for Non-Discrimination and Equal Treatment related to HIV, led by the Ministry of Health, Consumer Affairs and Social Welfare. This pact explains that women have biological differences that cause them to be at least twice as likely to contract HIV. But that’s not all: it specifies that various social, economic, and cultural factors place women in a “greater risk situation” regarding this virus.
Vulnerability factors
Experiencing gender-based violence, living in a patriarchal society, family situation, or limited access to education and work are conditions that increase the likelihood of contracting HIV. This is outlined in a situation report prepared by UNAIDS together with the WHO on HIV. For example, they mention that when a young woman is expelled from her family, she faces social marginalization and, in most cases, resorts to sexual exploitation to survive, increasing her vulnerability to HIV infection. Additionally, they explain that in countries with high HIV incidence, intimate partner violence can increase a woman’s likelihood of contracting the virus by up to 50%.
Another factor is difficulty accessing education and the labor market. As detailed in the research, women without education or with low educational levels often end up in poorly paid jobs that lead to low income. This economic situation causes women to depend on their families or, if alone, to live with poor quality of life and deteriorating health, raising the risk of contracting HIV and later AIDS. However, the study also indicates that many women who manage to access education encounter a system that reinforces patriarchal culture and discriminatory stereotypes that limit teaching about sexual health and HIV prevention methods.
Adding to all this is the place of birth of women, which is one of the greatest vulnerability variables for contracting HIV, as highlighted in the UNAIDS study ‘At Risk’. In Spain, as various studies show, similar to most European countries, the percentage of women who contract HIV is lower than that of men. This gap narrows in Sub-Saharan African countries, where women and adolescent girls are the most affected by this virus because a new infection is recorded every two minutes, and it is estimated they have three times the likelihood of contracting the virus compared to men.
Beyond the African continent is India, which has become one of the countries with the highest number of HIV cases among women, according to the United Nations. Rural areas are where cases grow fastest, attributed to a lack of information and awareness among the population. A program by the Vicente Ferrer Foundation has pointed out another key factor, denouncing that in “rural areas, women suffer from malnutrition because, according to traditions, they eat last.” These customs affect girls from childhood, making “a girl less well-nourished than a boy,” and this nutritional deficit hinders the effectiveness of antiretroviral treatment, thereby increasing mortality rates.
Delayed detection
According to the Advisory Committee on Vaccines of the Spanish Pediatric Association (AEP), “there is no other disease where stigma and social discrimination are as decisive as AIDS.” This context, combined with misinformation, causes delays in testing and HIV diagnosis. So much so that the Ministry of Health reports that in Spain, 13% of people living with HIV do not know they are infected. During the ‘Juntas y VIHvas’ conference coordinated by CESIDA, speaker and doctor at Valencia’s University Clinical Hospital, María José Galindo, highlighted that “women with HIV in Spain are diagnosed later and in worse immunological condition.” She also added that “most clinical trials are conducted on men and extrapolated to women, even though drugs affect them very differently.” The caregiver role that society places on women means that “many times they neglect themselves and their treatment.”

At the International AIDS Conference, UNAIDS has raised the alarm, warning that “last year’s new data are terrifying” with four new cases per minute, totaling 1.5 million new infections and over 650,000 deaths. To reverse these figures, the WHO is working on the 95-95-95 plan, which aims by 2030 to have 95% of people living with HIV diagnosed, 95% receiving treatment, and 95% achieving an undetectable viral load all while maintaining 0% discrimination. Despite this, UNAIDS calls for increased investment and equitable distribution of resources to avoid reaching one of the most dangerous moments in the fight against HIV. Ultimately, over 80% of cases occur in low-income countries, where women are the most vulnerable group.
Useful links:
Keys to understanding the accelerated action approach to end the AIDS epidemic by 2030. https://www.unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_
2022 Global AIDS Report ‘At Risk’ by UNAIDS. https://www.unaids.org/sites/default/files/media_asset/2022-global-aids-update-summary_es.pdf
Study by the Ministry of Health on the Epidemiological Surveillance of HIV and AIDS in Spain in 2020. https://www.sanidad.gob.es/ciudadanos/enfLesiones/enfTransmisibles/sida/vigilancia/
gender-based violence: an approach from social determinants by UNAIDS and WHO.. https://www.paho.org/gut/dmdocuments/
INFORMEDESITUACION.VIH%20y%20VBG.PDF
The hospital of the Vicente Ferrer Foundation, a reference center throughout India. https://fundacionvicenteferrer.org/es/blog/el-hospital-de-la-fundacion-vicente-ferrer-un-centro-de-referencia-en-toda-la-india
Due to factors such as origin and difficulties accessing education and work, the most affected are those living in Sub-Saharan Africa and India.
In mid-1981, the first cases of the Human Immunodeficiency Virus (HIV) were diagnosed worldwide. It started in the United States, and a few months later the first case was reported in Spain, eventually becoming a global pandemic. As noted by the World Health Organization (WHO), this virus attacks the immune system, and treatments can prevent its progression and the development of Acquired Immunodeficiency Syndrome (AIDS).
Since the first cases recorded in the 1980s according to a report by the United Nations’ UNAIDS it is estimated that 78 million people worldwide have contracted HIV, with nearly 37 million active cases currently. In Spain, the Ministry of Health indicates that around 88,700 AIDS cases have been reported in total, and there are currently between 140,000 and 170,000 people living with HIV.
The peak of registered cases occurred in the mid-1990s, and thanks to antiretroviral treatment, the numbers have decreased “progressively,” although this decline has slowed in recent years. Data from the Ministry of Health show 1,925 HIV cases in 2020, with approximately 15% being women under 35 years old the age group with the highest incidence. Medical experts point out that the disease “does not develop the same way in women and men.” In women, complications may include a higher risk of cervical cancer, menstrual cycle problems, increased likelihood of developing osteoporosis, earlier onset of menopause, or risk of transmission to the fetus during pregnancy.
The latest epidemiological surveillance study on HIV and AIDS in Spain shows an increase in virus transmission through heterosexual relationships, with 80.5% of new cases in women occurring in this type of relationship. To curb these figures, work is underway on the Social Pact for Non-Discrimination and Equal Treatment related to HIV, led by the Ministry of Health, Consumer Affairs and Social Welfare. This pact explains that women have biological differences that cause them to be at least twice as likely to contract HIV. But that’s not all: it specifies that various social, economic, and cultural factors place women in a “greater risk situation” regarding this virus.
Vulnerability factors
Experiencing gender-based violence, living in a patriarchal society, family situation, or limited access to education and work are conditions that increase the likelihood of contracting HIV. This is outlined in a situation report prepared by UNAIDS together with the WHO on HIV. For example, they mention that when a young woman is expelled from her family, she faces social marginalization and, in most cases, resorts to sexual exploitation to survive, increasing her vulnerability to HIV infection. Additionally, they explain that in countries with high HIV incidence, intimate partner violence can increase a woman’s likelihood of contracting the virus by up to 50%.
Another factor is difficulty accessing education and the labor market. As detailed in the research, women without education or with low educational levels often end up in poorly paid jobs that lead to low income. This economic situation causes women to depend on their families or, if alone, to live with poor quality of life and deteriorating health, raising the risk of contracting HIV and later AIDS. However, the study also indicates that many women who manage to access education encounter a system that reinforces patriarchal culture and discriminatory stereotypes that limit teaching about sexual health and HIV prevention methods.
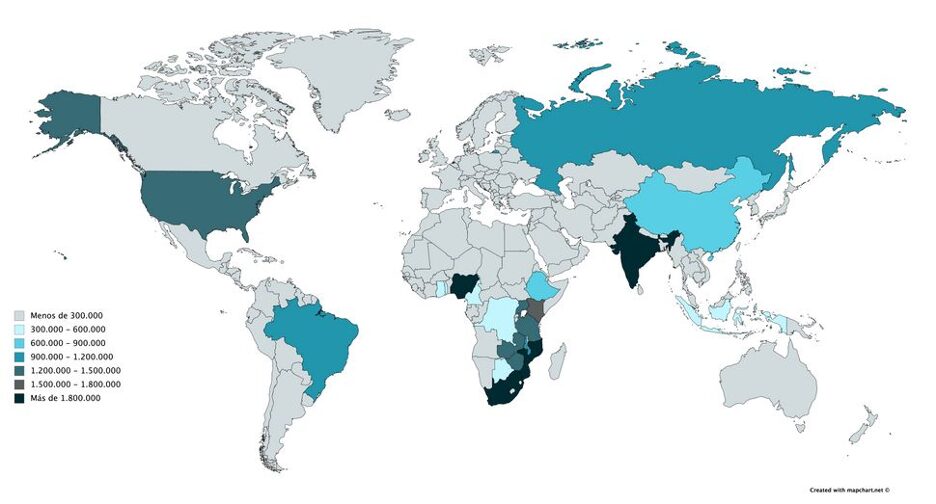
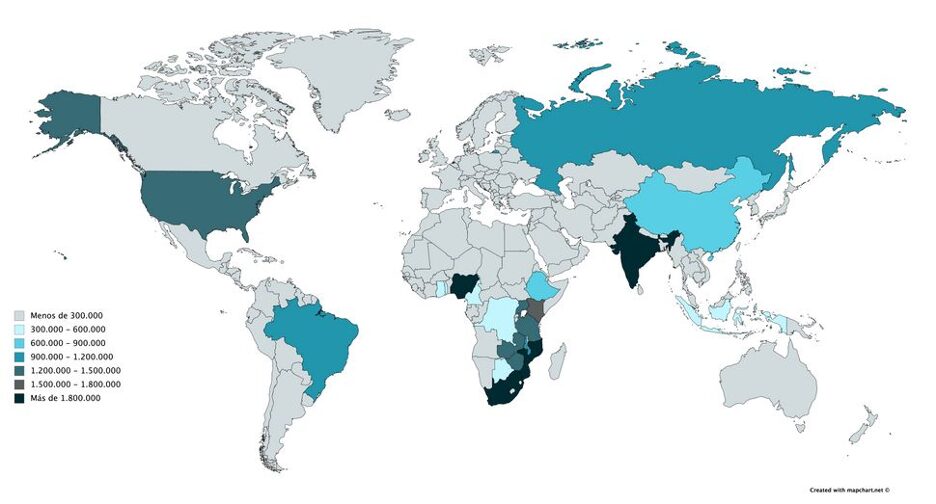
Adding to all this is the place of birth of women, which is one of the greatest vulnerability variables for contracting HIV, as highlighted in the UNAIDS study ‘At Risk’. In Spain, as various studies show, similar to most European countries, the percentage of women who contract HIV is lower than that of men. This gap narrows in Sub-Saharan African countries, where women and adolescent girls are the most affected by this virus because a new infection is recorded every two minutes, and it is estimated they have three times the likelihood of contracting the virus compared to men.
Beyond the African continent is India, which has become one of the countries with the highest number of HIV cases among women, according to the United Nations. Rural areas are where cases grow fastest, attributed to a lack of information and awareness among the population. A program by the Vicente Ferrer Foundation has pointed out another key factor, denouncing that in “rural areas, women suffer from malnutrition because, according to traditions, they eat last.” These customs affect girls from childhood, making “a girl less well-nourished than a boy,” and this nutritional deficit hinders the effectiveness of antiretroviral treatment, thereby increasing mortality rates.
Delayed detection
According to the Advisory Committee on Vaccines of the Spanish Pediatric Association (AEP), “there is no other disease where stigma and social discrimination are as decisive as AIDS.” This context, combined with misinformation, causes delays in testing and HIV diagnosis. So much so that the Ministry of Health reports that in Spain, 13% of people living with HIV do not know they are infected. During the ‘Juntas y VIHvas’ conference coordinated by CESIDA, speaker and doctor at Valencia’s University Clinical Hospital, María José Galindo, highlighted that “women with HIV in Spain are diagnosed later and in worse immunological condition.” She also added that “most clinical trials are conducted on men and extrapolated to women, even though drugs affect them very differently.” The caregiver role that society places on women means that “many times they neglect themselves and their treatment.”

At the International AIDS Conference, UNAIDS has raised the alarm, warning that “last year’s new data are terrifying” with four new cases per minute, totaling 1.5 million new infections and over 650,000 deaths. To reverse these figures, the WHO is working on the 95-95-95 plan, which aims by 2030 to have 95% of people living with HIV diagnosed, 95% receiving treatment, and 95% achieving an undetectable viral load all while maintaining 0% discrimination. Despite this, UNAIDS calls for increased investment and equitable distribution of resources to avoid reaching one of the most dangerous moments in the fight against HIV. Ultimately, over 80% of cases occur in low-income countries, where women are the most vulnerable group.
Useful links:
Keys to understanding the accelerated action approach to end the AIDS epidemic by 2030. https://www.unaids.org/
sites/default/files/media_asset
Understanding_FastTrack_es.pdf
2022 Global AIDS Report ‘At Risk’ by UNAIDS. https://
default/files/media_asset/2022-global-aids-update-summary_es.pdf
Study by the Ministry of Health on the Epidemiological Surveillance of HIV and AIDS in Spain in 2020. https://www.sanidad.gob.es/
Situation report on HIV and gender-based violence: an approach from social determinants by UNAIDS and WHO. https://www.paho.org/gut
The hospital of the Vicente Ferrer Foundation, a reference center throughout India. https://fundacionvicenteferrer
.org/es/blog/el-hospital-de-la-fundacion-vicente-ferrer-un-centro-de-referencia-en-toda-la-india

